When you’re hurting, it’s tempting to take the fastest route to relief. And in sports medicine, few interventions are as common, or as misunderstood, as the cortisone shot.
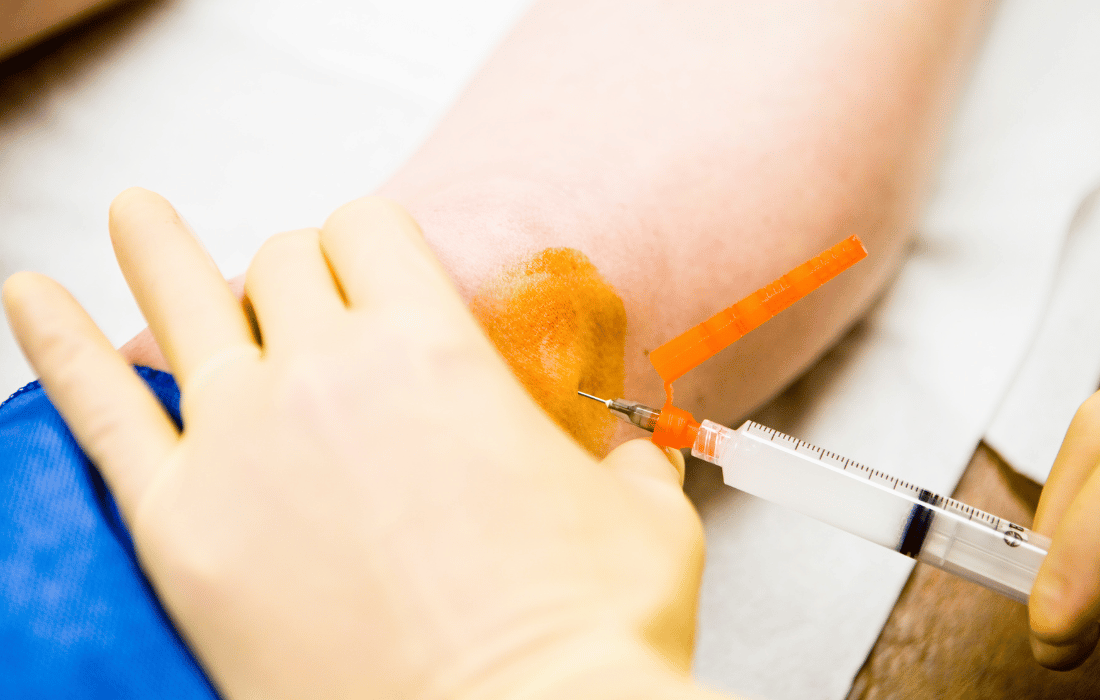
Used to treat inflammation and pain in joints, tendons, and soft tissue, cortisone injections are a go-to for many doctors, trainers, and athletes. But for all their short-term magic, these shots carry long-term consequences that aren’t always discussed.
From CrossFitters to climbers, MMA fighters to marathoners, athletes need to understand what they’re really signing up for when they opt for a quick fix. Because sometimes, what seems like a shortcut is actually a slow detour to more injury, less resilience, and chronic damage.
What Is Cortisone, Really?
 Cortisone is a type of corticosteroid, a powerful anti-inflammatory hormone that can be injected directly into joints or tissue to reduce swelling and pain. It’s not a painkiller in the way ibuprofen or acetaminophen is – instead, it suppresses the body’s inflammatory response.
Cortisone is a type of corticosteroid, a powerful anti-inflammatory hormone that can be injected directly into joints or tissue to reduce swelling and pain. It’s not a painkiller in the way ibuprofen or acetaminophen is – instead, it suppresses the body’s inflammatory response.
This makes it useful in treating conditions like:
- Tendinitis (Achilles, patellar, rotator cuff)
- Bursitis
- Plantar fasciitis
- Joint arthritis (knee, hip, shoulder)
- Tennis elbow or golfer’s elbow
Cortisone can reduce swelling in a matter of days and allow an athlete to return to training or competition quickly, which is why it’s so appealing.
But this relief comes with some costs.
The Catch: What Cortisone Doesn’t Do
Cortisone doesn’t address the root cause of your pain; it just mutes it.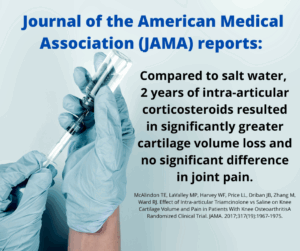
In many cases, pain and inflammation are the body’s adaptive response to overuse or micro-damage. Numbing the pain might allow an athlete to return to play, but without healing the underlying issue, they risk deeper, more permanent damage.
Worse, repeated cortisone use can weaken tissue.
Documented Risks
- Tendon degeneration or rupture (especially Achilles and patellar tendons)
- Cartilage loss in joints, accelerating osteoarthritis
- Delayed healing
- Weakened ligaments
- Fat atrophy and skin discoloration at the injection site
This isn’t fear-mongering. Peer-reviewed studies show that repeated cortisone injections can actually worsen structural outcomes over time, especially when used within short intervals or injected directly into weight-bearing joints.
Case Study: The Athlete Who Trains Through It
Take a grappler dealing with elbow tendinitis. They get a cortisone shot to reduce pain and inflammation. It works. They’re back on the mats in two days. But since the underlying friction and joint instability haven’t been addressed, they keep training at full throttle.
Fast-forward three months: that elbow tendinitis has become tendon degeneration, maybe even a partial tear. Recovery will now require months of rest and rehab, far more costly than taking two weeks off and treating it conservatively up front.
Cortisone creates a false sense of readiness. And in sports, false confidence is dangerous.
One Shot? Maybe. Multiple? Think Again.
Medical consensus is shifting. For acute inflammation, a single cortisone injection may be helpful, especially for athletes with a competition on the line. But repeat injections, especially within 3–6 months, are increasingly discouraged.
In fact, many orthopedic clinics now place limits on cortisone injections:
- No more than 3 per year in the same joint
- Spaced out by at least 6–8 weeks
- Used only in combination with corrective rehab or lifestyle change
Still, there are exceptions and edge cases – every injury is different. But the bigger issue is that most athletes aren’t told about these risks up front.
Safer Alternatives for Athletes
If you’re dealing with inflammation, don’t rush for the needle. Here are smart alternatives that support healing instead of masking symptoms:
Load Management
Deload or modify your training – not just volume but type. Switching to isometric holds or eccentric loading can rebuild tissue integrity without aggravating injuries.
Manual Therapy & Mobility Work
Techniques like active release therapy (ART), fascial stretch, and targeted mobility drills can free up impingements and improve biomechanics.
Red Light Therapy (Photobiomodulation)
Backed by growing evidence, red light therapy promotes cellular repair, reduces inflammation, and enhances collagen synthesis.
reduces inflammation, and enhances collagen synthesis.
PRP (Platelet-Rich Plasma) Injections
A regenerative option using your own blood platelets to stimulate healing. Slower than cortisone but more aligned with tissue repair.
Anti-Inflammatory Nutrition
Cut seed oils and refined sugars. Increase omega-3s, turmeric, ginger, collagen, and gelatin-rich foods to support tendon and joint health from the inside out.
EMF Reduction
For some, chronic inflammation may also be influenced by non-obvious stressors. Limiting EMF exposure, especially during sleep and recovery, can improve cellular recovery and reduce background stress that contributes to inflammatory load.
Aires for Athletes

For athletes exploring EMF reduction as part of their anti-inflammatory strategy, Aires offers scientifically validated solutions that help mitigate the physiological stress of electromagnetic fields. Their devices are designed to harmonize the chaotic signals emitted by phones, tablets, Wi-Fi routers, and other sources of daily radiation.
While EMFs are still an emerging area of study in sports recovery, reducing this invisible load may support nervous system balance, better sleep, and cellular repair, especially during high training periods or injury recovery.
When Is Cortisone Justified?
There is, potentially, a time and place for cortisone, particularly:
- When pain is crippling and acute
- When the athlete has a short window before a key event
- When used once and paired with a longer-term rehab plan
The danger comes when it’s viewed as a fix, not a tool. Used without context or care, cortisone is like putting duct tape over a check-engine light.
The Hidden Cost of Playing Through Pain
Cortisone fits neatly into a larger pattern in sports: ignoring smallproblems until they become big ones. The cultural emphasis on toughness, pushing through, and “no pain, no gain” often overshadows smarter, more sustainable practices.
But every time pain is masked rather than investigated, it deepens the disconnect between athlete and body. When pain is used as a signal, not an inconvenience, it becomes a guide for longevity, not a threat to performance.

A Culture Shift Is Needed
Athletic culture still rewards pushing through pain, but longevity is the new flex. The strongest athletes are the ones who stay in the game for decades, not just months. And the healthiest bodies are the ones allowed to heal, not hacked for short-term gains.
Coaches, clinics, and athletes need to shift the conversation from “How fast can I get back?” to “What’s going to keep me strong ten years from now?”
Because in the long run, choosing patience over the needle might just be the most high-performance move you can make.